[Check the byline, thanks! /~Rayne]
Funny enough, this COVID-19 post originally came about because of one of my family members.
They sent me a link to an op-ed from the Detroit News — the more conservative of the two major Detroit-based papers in this state — in which the author took Michigan’s Gov. Gretchen Whitmer to task because the state’s Department of Licensing and Regulatory Affairs clamped down on off-label prescriptions of an antimalarial drug.
“Any thoughts on the mandate against hydroxychloroquine?” they asked along with the link.
“Oh no,” I replied, “the author is going to regret writing that op-ed.”
They really had no idea what they were writing about. But then Trump doesn’t either.
~ ~ ~
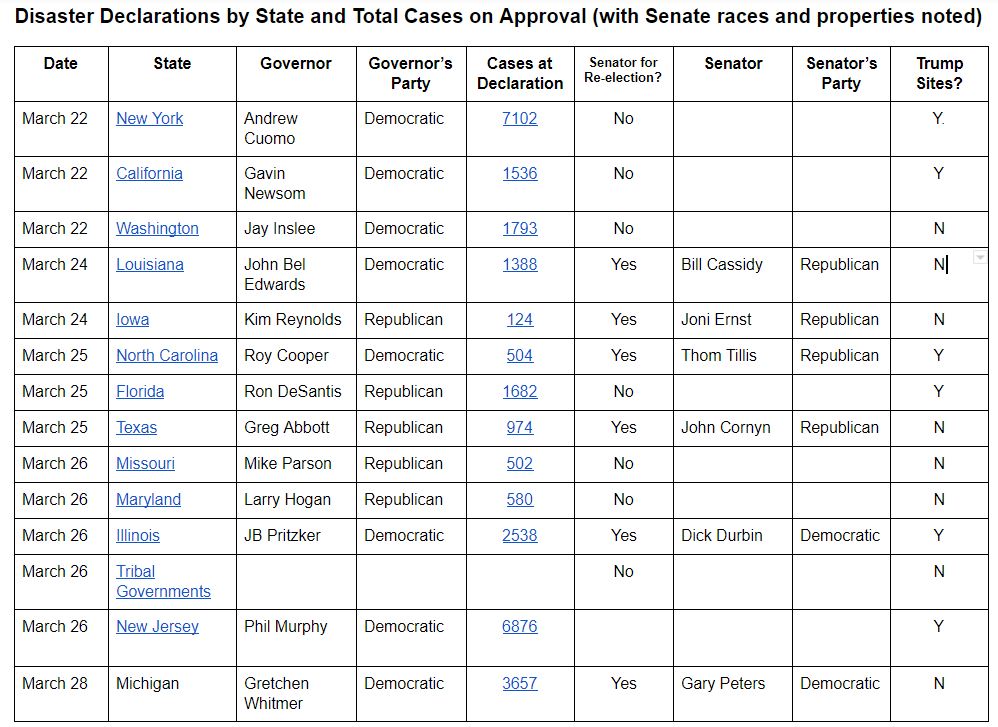
We’re desperate. Trump and his minions don’t want to admit it, carrying on with Trump’s daily self-fluffing at the podium in front of his narcissistic supply, I mean, select White House press pool as if everything is under control.
We the public know it’s not. On Wednesday March 25, actor and activist George Takei pointed out a person died of COVID-19 in New York City every six minutes the previous day. The numbers have only grown worse.
We are that measurably desperate.
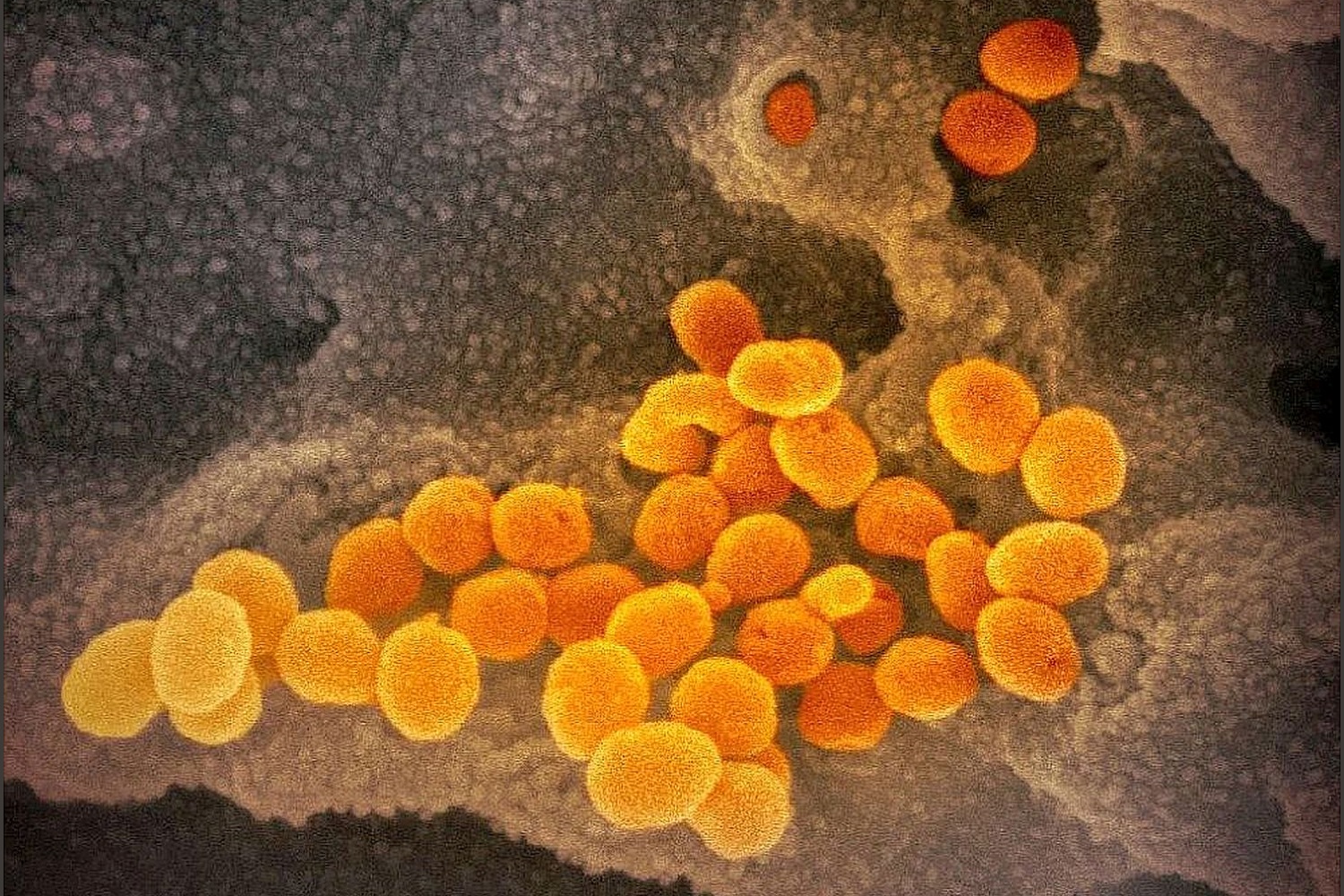
We’re grabbing at any kind of research, peer-reviewed and not, to find a way to shut down this fire hose of death because the other realistic alternative is at least 18 months of alternating levels of social distancing until a vaccine for COVID-19 has made it through multiple trials.
In a previous post I did homework and laid out some of the off-label approaches which have been taken in other equally desperate countries — like the antiviral remdesivir and the rheumatoid arthritis medication tocilizumab. These are in studies and haven’t been approved for use against COVID-19. We can only hope that other countries’ desperate, compassionate use of drugs off-label will add to the body of knowledge we have about effective treatments between now and the vaccine to come.
Our desperation makes us sloppy. We forget that what looks too good to be true often is just that.
Like the combined drug cocktail hydroxychloroquine and azithromycin.
~ ~ ~
Back on March 13 while writing about drug therapies in research, I wrote:
A number of existing drugs have been revisited for repurposing against COVID-19 instead of their original intended purpose. Antiviral remdesivir and antimalarial chloroquine are among them.
Chinese researchers posted a paper about in vitro results, not peer reviewed (at least I didn’t see that it was).
There’s a paper about chloroquine alone; in vitro studies suggest it may work against COVID-19. Chinese researchers have a number of in vivo studies in progress, but no data has been released.
Chloroquine by itself as an effective therapy would be a miracle in that it’s an old drug now off patent and available as a generic, super cheap to produce. Can’t imagine Big Pharma would like this. But we won’t even face this conflict if we don’t get data from in vivo studies.
Data. We needed data from peer-reviewed in vivo studies before any pronouncement could be made about the antimalarial medication as a therapy for COVID-19.
Published March 2 in Science Direct, a commentary by researchers at Aix Marseille University said essentially the same thing after examining an announcement by Chinese researchers that chloroquine phosphate was better than a control in treating SARS-CoV-2 (COVID-19) pneumonia — an announcement which had no supporting data:
In conclusion, the option of using chloroquine in the treatment of SARS-CoV-2 should be examined with attention in light of the recent promising announcements, but also of the potential detrimental effect of the drug observed in previous attempts to treat acute viral diseases. We urge Chinese scientists to report the interim trial results currently running in China as soon as they are available. This should be preferentially done in a peer-reviewed publication with detailed information to allow the international scientific community to analyse the results, to confirm in prospective trials the efficacy of the proposed treatment and to guide future clinical practice.
(Emphasis mine.)
These researchers are literally begging the Chinese researchers to provide data as soon as possible, after noting that while hydroxychloroquine’s precursor chloroquine appeared effective as an antiviral in vitro against different viruses, it has shown no benefit in animal models. (They also noted in a study of its efficacy against chikungunya virus, chloroquine actual “enhanced” viral replication in animal models. Not good.)
A study was published around the March 24 but reports said it was unfavorable for the antimalarial. (I haven’t been able to get my hands on the study; the link from each news source citing it has failed.) The size of the group studied was very small — only 30 patients with a control group of 15.
And yet sandwiched in time between the first Chinese study and this most recent one was another one submitted for publication on March 17:
Gautret et al. (2020) Hydroxychloroquine and azithromycin as a treatment of
COVID‐19: results of an open‐label non‐randomized clinical trial. International Journal of
Antimicrobial Agents – In Press 17 March 2020 – DOI : 10.1016/j.ijantimicag.2020.105949
https://www.mediterranee-infection.com/wp content/uploads/2020/03/Hydroxychloroquine_final_DOI_IJAA.pdf
The researchers from Aix Marseille University made no mention of this study though it must have been underway in their own backyard, so to speak.
No one noticed this — the dog that didn’t bark.
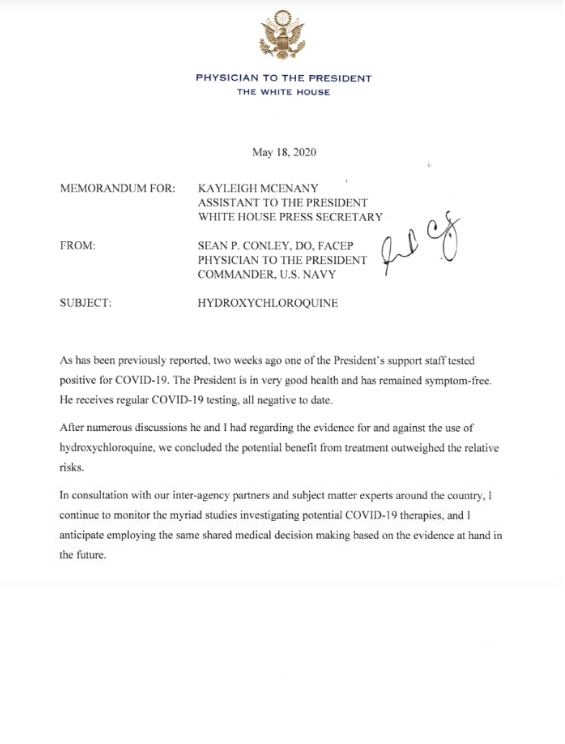
Meanwhile, on March 19, Trump talked about hydroxychloroquine from the podium during a briefing before a White House press pool. He not only mentioned it in glowing terms but he tweeted about it. Mike Pence also promoted the antimalarial two days later.
On March 24 an Arizona man died and his wife was hospitalized after taking hydroxychloroquine’s precursor, chloroquine — used to maintain their fish tank — having heard Trump talk about it so positively. The couple poisoned themselves; Trump scored two casualties with his misinformation.
~ ~ ~
A critical threat to U.S. health security is its monoculture — specifically, its complete investment in English excluding other languages. Back when we worried about Zika virus posing a threat to Americans traveling to South America and when Zika arrived in Florida, we were combing through research from other countries. The Chinese fortunately published much of their work in both Mandarin and English, but Brazil had a considerable amount in Portuguese. Their work was ignored in favor of less credible work which appeared in English.
This same dynamic is at work with regard to potential drug therapies — hydroxychloroquine in particular.
The study Gautret et al. (2020) was published in French and English, you’ll note. Many people picked up on it because it was so accessible.
What wasn’t picked up readily was the problems with an affiliated researcher. Many reported problems have been documented online where the world can read them, in of all places, Wikipedia.
But that’s Wikipedia France — a different address than we use in the U.S., published in French.
See: https://fr.wikipedia.org/wiki/Didier_Raoult
Use Google Translate and read the section on COVID-19. The translation isn’t entirely smooth but it does well enough for the average English speaker to figure out Raoult is a character.
He also has a history of sexual harassment and possible abuse according to a number of accusers, also documented in this Wikipedia entry.
(I’ve scraped that entry and translated it out of concerns it might change over time. You can read the portion of the French Wikipedia entry on Raoult and COVID-19 at this link. You can compare it against the Wikipedia page’s editing history though you’ll need to reverse translate it.)
It could be said in the MeToo age that many accused abusers are competent at their professions and are simply jerks when it comes to managing their attitude toward co-workers. But in Raoult’s case the accusations are smoke and where there’s smoke there’s an ethical fire.
It seems Raoult’s research has had a problem with data which looks artificial in at least two other studies, noted during peer review.
He’d previously been banned from publishing in microbiology journals.
Complaints about a hostile work environment in his lab do not offer reassurance about the credibility of his work. Were subordinates pressured for results?
It also seems odd this one study from France has been relied on so heavily by others, when the underlying drug is manufactured by a French manufacturer (though not the only company which does).
None of this passes the smell test.
Gautret et al. also didn’t pass the sniff test with the journal in which it was published though it did not retract the study:
The April 3, 2020, notice, from the International Journal of Antimicrobial Agents, states that the March 20 article, “Hydroxychloroquine and azithromycin as a treatment of Covid-19: results of an open-label non-randomized clinical trial”
does not meet the [International Society of Antimicrobial Chemotherapy’s] expected standard, especially relating to the lack of better explanations of the inclusion criteria and the triage of patients to ensure patient safety.
The notice, which is from the ISAC and not the journal itself, is a bit ambiguous. The society says it “shares the concerns” about the paper, but it doesn’t appear to be taking additional action.
It’s unclear what took the journal nearly a month to make this statement of doubt. Because it hasn’t been retracted references are still made to Gautret et al. (2020).
~ ~ ~
Studies to date on hydroxychloroquine or its precursor chloroquine have been small or flawed; the merits of these antimalarials were thin to begin with.
Zumla, A., Chan, J., Azhar, E. et al. Coronaviruses — drug discovery and therapeutic options. Nat Rev Drug Discov 15, 327–347 (2016).
Published: 12 February 2016
https://doi.org/10.1038/nrd.2015.37
https://rdcu.be/b3uhd
An excerpt from this review of drug therapies notes chloroquine had limited promise against SARS-CoV-1:
…Chloroquine is an anti-malarial drug that sequesters protons into lysosomes to increase the intracellular pH. It has broad-spectrum antiviral activities against numerous CoVs (SARS-CoV, MERS-CoV, HCoV-229E and HCoV-OC43) and other RNA viruses in vitro 123, 210, 211, 212, 213, 214. However, it did not substantially reduce viral replication in SARS-CoV-infected mice, possibly because the cell surface pathway was not simultaneously blocked. …
This study of antiviral remdesivir with antimalarial chloroquine was in vitro, not in vivo:
Wang, M., Cao, R., Zhang, L. et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 30, 269–271 (2020).
Published: 04 February 2020
https://doi.org/10.1038/s41422-020-0282-0
Remdesivir may act alone as antiviral. Conclusion is that these two drugs “should be assessed in human patients suffering from the novel coronavirus disease.” The drugs were assessed but not employed as a protocol.
This next study is again in vitro, not in vivo:
Liu, J., Cao, R., Xu, M. et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov 6, 16 (2020).
Published: 18 March 2020
https://doi.org/10.1038/s41421-020-0156-0
https://www.nature.com/articles/s41421-020-0156-0
Its conclusion calls for more testing, while implying hydroxychloroquine’s use would be better as an anti-inflammatory during cytokine storm though this study didn’t examine its anti-inflammatory effects:
…HCQ is a safe and successful anti-inflammatory agent that has been used extensively in autoimmune diseases and can significantly decrease the production of cytokines and, in particular, pro-inflammatory factors. … In combination with its anti-inflammatory function, we predict that the drug has a good potential to combat the disease. This possibility awaits confirmation by clinical trials. We need to point out, although HCQ is less toxic than CQ, prolonged and overdose usage can still cause poisoning. And the relatively low SI of HCQ requires careful designing and conducting of clinical trials to achieve efficient and safe control of the SARS-CoV-2 infection.
Hydroxychloroquine is toxic and it needs carefully designed clinical trials — this prediction of its “good potential” is happy talk until there’s data to prove its effectiveness for its intended purpose.
A pre-proof study about the two-drug hydroxychloroquine and azithromycin cocktail published on March 30 is small but makes a more declarative statement right in its title:
Molina JM, Delaugerre C, Goff JL, Mela-Lima B, Ponscarme D,
Goldwirt L, de Castro N, No Evidence of Rapid Antiviral Clearance or Clinical Benefit with the
Combination of Hydroxychloroquine and Azithromycin in Patients with Severe COVID-19
Infection, Medecine et Maladies Infectieuses (2020),
doi: https://doi.org/10.1016/j.medmal.2020.03.006
https://www.sciencedirect.com/science/article/pii/S0399077X20300858
The summary:
In summary, despite a reported antiviral activity of chloroquine against COVID-19 in vitro, we found no evidence of a strong antiviral activity or clinical benefit of the combination of hydroxychloroquine and azithromycin for the treatment of our hospitalized patients with severe COVID-19. Ongoing randomized clinical trials with hydroxychloroquine should provide a definitive answer regarding the alleged efficacy of this combination and will assess its safety.
This study was in vivo, using the same dosing regimen reported by Gautret et
al. study on a cohort of patients similar to the same study. The results were unsatisfactory:
At the time of treatment initiation, 10/11 had fever and received nasal oxygen therapy. Within 5 days, one patient died, two were transferred to the ICU. In one patient, hydroxychloroquine and azithromycin were discontinued after 4 days because of a prolongation of the QT interval from 405 ms before treatment to 460 and 470 ms under the combination. Mean through blood concentration of hydroxychloroquine was 678 ng/mL (range: 381-891) at days 3-7 after treatment initiation.
Nor had the virus been cleared 5-6 days after treatment began in 8 of 10 surviving patients. The study’s authors made a point to compare their findings against the Gautret et al. study:
These virologic results stand in contrast with those reported by Gautret et al. and cast doubts about the strong antiviral efficacy of this combination. Furthermore, in their report Gautret et al also reported one death and three transfers to the ICU among the 26 patients who received hydroxychloroquine, also underlining the poor clinical outcome with this combination.
Hydroxychloroquine doesn’t work against SARS-CoV-19 even when paired with the antibiotic azithromycin, but a larger, randomized clinical trial with appropriate controls is still necessary to beat it through the heads of people pushing this therapy.
~ ~ ~
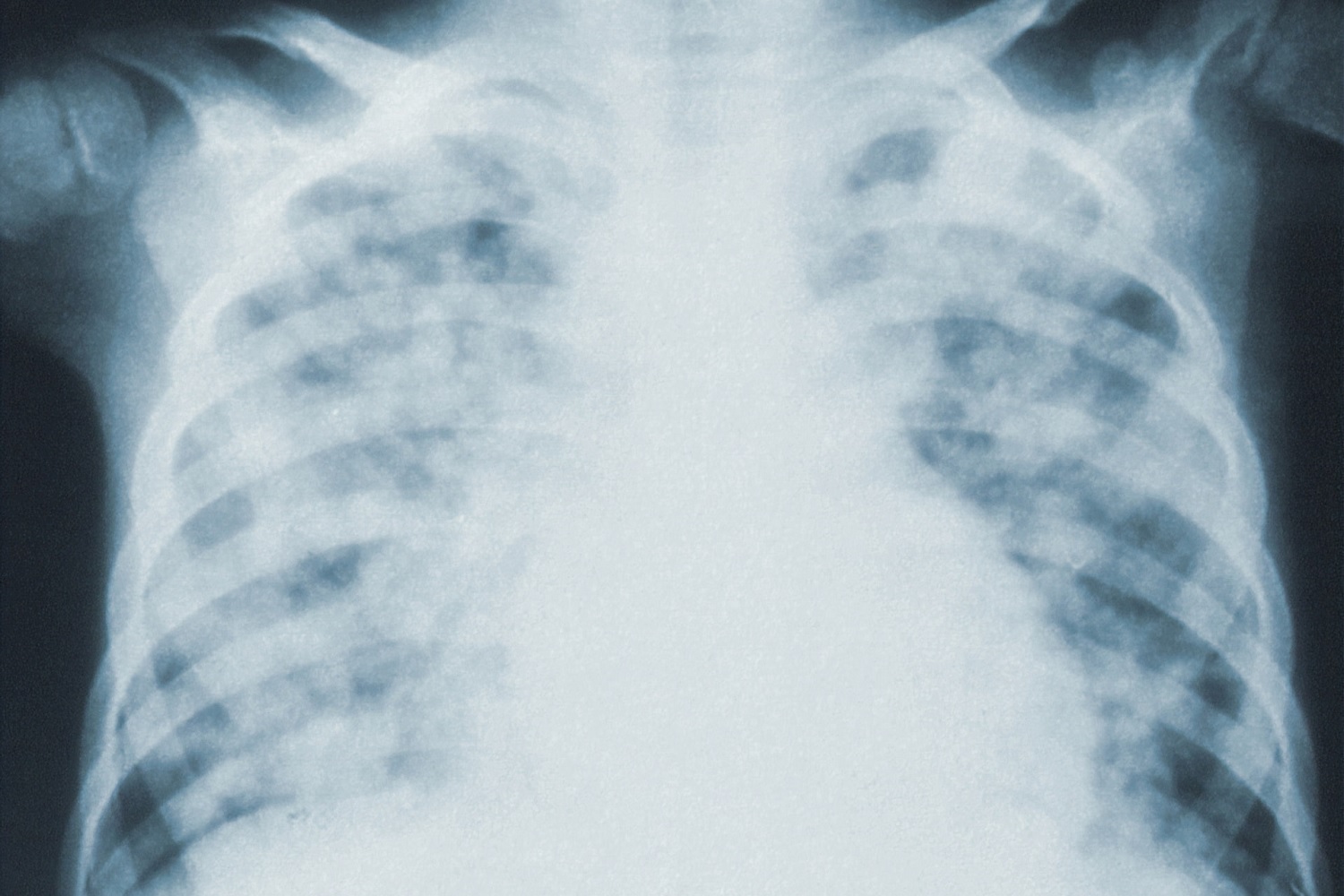
But out of desperation, hospitals have been using hydroxychloroquine anyhow, only to discover it doesn’t work against COVID-19 — it may even make patients sick.
That last French study above squelched further use of hydroxychloroquine at the St. Louis Hospital in Paris.
Hospitals in Sweden stopped using it after negative effects (open link in Chrome and use Google Translate to read in English) including impaired vision.
On Sunday, Dr. Sanjum S. Sethi, Vascular Medicine and Interventional Cardiology Columbia University Irving Medical Center, shared that ALL patients treated in the ICU for COVID-19 have received hydroxychloroquine:
Dr. Sethi doesn’t say how many patients have been treated with the drug so far — there could be as many as 1,000 patients in ICU at one time based on a newsletter by Surgeon-in-Chief Craig R. Smith, MD for NYP/CUIMC — but it didn’t work for severe-to-critical patients in ICU.
Which means the Chinese researchers’ suggestion that hydroxychloroquine’s anti-inflammatory qualities may help with cytokine storms didn’t pan out.
~ ~ ~
Meanwhile, Trump continues to tout hydroxychloroquine, as does his best buddy in Brazil, Jair Bolsonaro.
Brazil, like other tropical countries has ongoing incidence of malaria. It’s endemic along the Amazon River and treated with chloroquine or hydroxychloroquine. The drug has also been used prophylatically.
And yet Brazil is experiencing a growth in COVID-19 cases even along the Amazon River, suggesting hydroxychloroquine or its precursor are not effective in the early stages of the disease, failing to fend off infection and contagious pre-symptomatic progression to mild, severe, and critical cases.
Further assessment is difficult because like Trump, Bolsonaro has undermined reporting and efforts to limit contagion.
Brazil’s Minister of Health Luiz Henrique Mandetta nearly lost his job late last week when he refused to authorize a protocol prescribing hydroxychloroquine for COVID-19 patients. A few doctors continued to press him on this after he survived a heated cabinet meeting in which this pharmaceutical was discussed.
Two days later a small study was published; chloroquine as therapy for COVID-19 patients had been halted early after more than 25% of the subjects died:
Borba M, Almeida Val F, Sousa Sampaio Vanderson, CloroCovid-19 Team, et al. Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: Preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (CloroCovid-19 Study)
Published: April 11, 2020
medRxiv 2020.04.07.20056424; doi: https://doi.org/10.1101/2020.04.07.20056424
https://www.medrxiv.org/content/10.1101/2020.04.07.20056424v1
~ ~ ~
The bottom line is that we are still without an effective pharmaceutical antiviral therapy, no matter what Trump says.
What he’s said from the podium has only encouraged risk-taking pushing past the limits of ethics guiding the practice of medicine and human experimentation. The Texas City nursing home administration who has dispensed hydroxychloroquine without advanced informed consent is a perfect example of ethics collapsing under Trump’s equally unethical practice of medicine and pharmaceutical lobbying from the presidential podium.
Though we know more now than we did at the beginning of March about hydrochloroquine as a tool for treating COVID-19 — and we know that no study to date has suggested the drug will be effective for a majority of COVID-19 patients — we still do not know why Trump is so invested in this generic medication.
Who told Trump this drug was an effective treatment for COVID-19?
Has someone continued to reinforce this fallacy though Dr. Fauci has yet to reverse his own professional opinion about hydroxychloroquine?
Who likewise sold Bolsonaro on this drug? It likely wasn’t Fox News though the network may have irresponsibly reinforced Trump’s lobbying for hydroxychloroquine.
Why are talking heads on Fox News still promoting this drug with impunity — like Laura Ingraham who is not a medical professional?
Why are other right-leaning pundits continuing to press for this drug though they do not have medical background, and while other experts continue to express doubts about hydroxychloroquine?
None of this makes sense; we lack information. As I said before, we need data from peer-reviewed in vivo studies before any pronouncement can be made about the antimalarial medication as a therapy for COVID-19.
And we need to know more about Trump’s reasons for promoting this drug while ignoring the risks hydroxychloroquine poses.
 For anybody that has read me here, or followed me on Twitter, you know I have maintained from the start that Fani Willis, and her “investigation” is a complete joke.
For anybody that has read me here, or followed me on Twitter, you know I have maintained from the start that Fani Willis, and her “investigation” is a complete joke.