Why Is The Battelle N95 Mask Sterilization Contract So Expensive?
Jim here.
Long time readers of the blog know that whenever I hear something about Battelle, my spidey senses go on full alert. Suffice it to say that the Battelle facility in West Jefferson, Ohio is one of only a few facilities on the planet that has both the expertise and the equipment to produce something like, say, a fully weaponized anthrax powder. So I’ve been going on alert the last few days as word has come out on Battelle’s process for sterilizing used N95 masks for re-use. West Jefferson is just outside Columbus, so I had a false alarm on Marcy’s post earlier today about the Washington Post needing to go to Columbus, but she wasn’t discussing Battelle.
Don’t get me wrong. I am fully in favor of anything that can be done to provide safe PPE to those on the front lines of the COVID-19 pandemic response. Finding safe ways to re-use these masks has to be one of the many approaches we must rely on while the masks are in such short supply. But when I finally started digging deeper into what is going on with the contract that the Defense Logistics Agency awarded to Battelle for this process, I was staggered by the total cost compared to what looks, on the surface, to be a straightforward, inexpensive already proven approach.
On April 13, the Department of Defense announced a $415 million contract to Battelle for N95 mask sterilization:
The Department of Defense’s Defense Logistics Agency, on behalf of the Department of Health & Human Services (HHS), has awarded a $415 million contract for 60 Battelle Memorial Institute Critical Care Decontamination Systems (CCDS), that can decontaminate up to 80,000 used N95 respirators per system per day, enabling mask reuse up to 20 times.
Spearheaded by the Department’s Joint Acquisition Task Force, six units have already been delivered to locations including two to New York, and one each to Columbus, Ohio, Boston, Chicago and Tacoma, providing the ability to sterilize 3.4 million masks a week, reducing the need for new masks by the same number.
All 60 systems will be available by early May for prioritization and distribution by FEMA and HHS. Once all are delivered, these 60 units will allow 4.8 million masks to be sterilized per day, almost 34 million per week.
‘I remain extremely proud of the selfless efforts of Department of Defense personnel who continue to do everything they can to help provide medical masks, test kits, medicine and meals to support America’s military, medical, emergency services and law enforcement professionals who are on the front lines and need them most,’ said Under Secretary of Defense Ellen Lord.
This procurement includes a service contract to cover operations and maintenance.
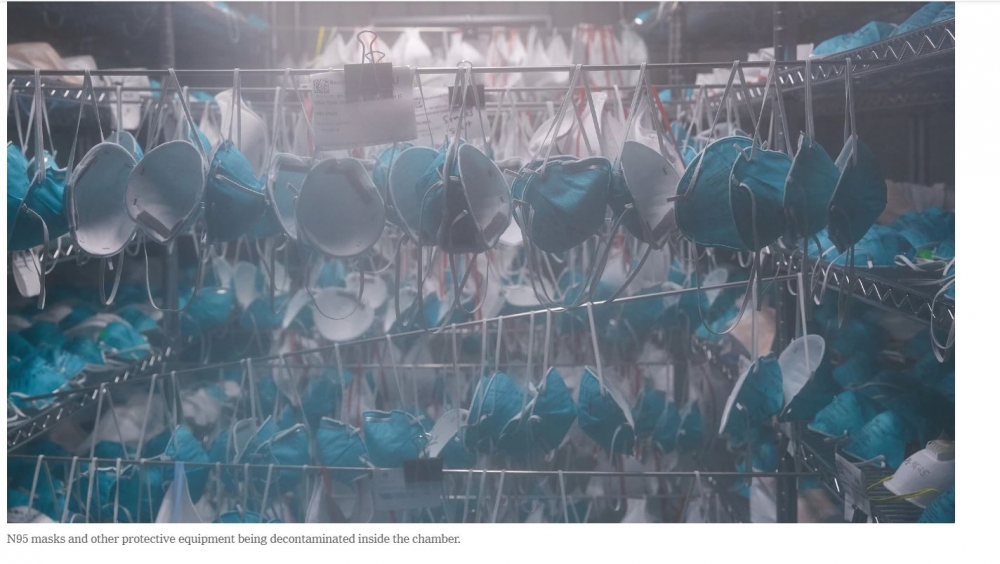
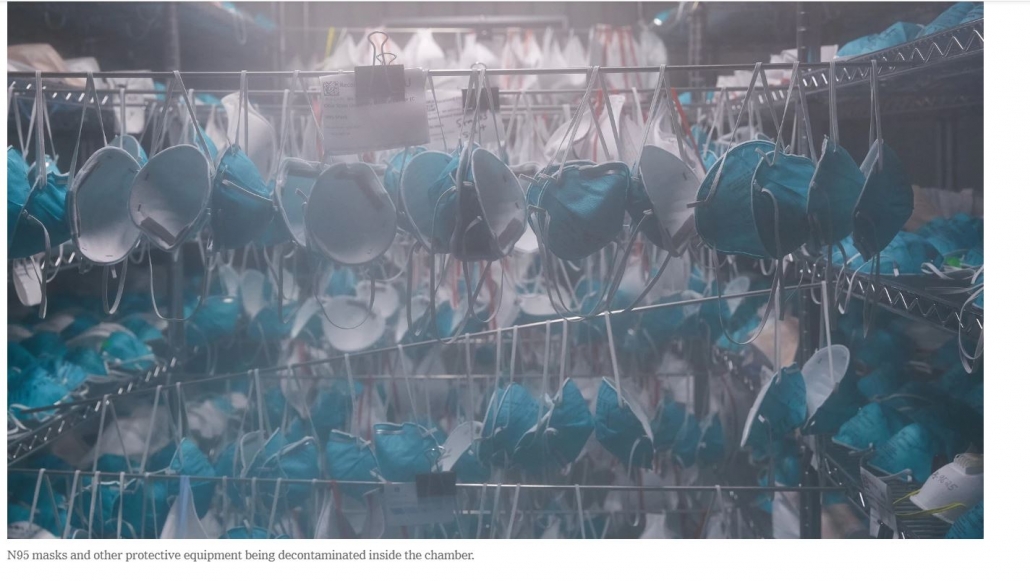
A couple of days earlier, on April 11, the New York Times visited Battelle and provided a photoessay on the Battelle process for sterilization. Here is a Times photo of masks hanging in one of the decontamination units. This photo is also the featured image for the post:
One thing that jumps out immediately is to notice that standard food/medical grade shelving is used in the unit. So at least that part isn’t very expensive. I am disturbed, though, by the “extra” rods between shelves that have masks hanging in a way that we can see multiple pairs of them closely nested, raising concern about circulation of the vapor used in the sterilization process. Just below the photo, the Times notes that workers take “care to avoid overlapping”. Okay, then, but I’m still nervous about those that look nested.
The sterilization process itself is carried out by hydrogen peroxide vapor (HPV). Of course, safety dictates that the chamber in which the masks are exposed to the vapor is perfectly sealed as vapors escaping would be toxic to the staff working around the chamber. Technology to inactivate the peroxide in the exhaust stream from the chamber is known, off the shelf technology and would be a part of the air handling for the chamber. Hydrogen peroxide itself is very inexpensive and is produced in bulk by the chemical industry.
Battelle already validated the process under a contract from FDA, with the final report issued in July of 2016 (thanks, Obama!). Here’s a partial screengrab from the report with a photo of the simple machine used to generate the HPV (gratuitous anthrax mention included for grins):
Sure enough, the Times found a very similar machine when they were at Battelle:
This is not a very complicated piece of machinery. I’m not sure of the full retail price, but I found a used “as is” listing for $4500. I’d be surprised if these are costing Battelle more than $20,000 per unit.
And the “chambers”? They’re shipping containers. Again, from the Times photos:
Also visible in this photo is very standard-looking air handling equipment.
So, making 60 units out of shipping containers, outfitting them with an HPV generator and air handling equipment doesn’t look very expensive to me at all when compared to the total value of the contract. It’s very hard to estimate more than $10-15 million in materials costs for 60 units.
The Times article provides an accessible description of the sterilization process. Here’s what happens in the chamber:
A contraption known as a vapor phase hydrogen peroxide generator, which looks like a washing machine with two hoses, is then used to circulate the colorless gas into and out of the room. During the first four hours, workers increase the humidity inside the chamber, causing the hydrogen peroxide to collect as condensation on the masks, neutralizing the coronavirus and other contaminants.
Over the next four hours, the gas is flushed out of the room. The teams then re-enter the chamber to inspect the masks and conduct spot tests for harmful levels of residual hydrogen peroxide. They then confirm that chemical indicator cards placed throughout the chamber have changed color — the sign of a successful decontamination.
The process itself is very labor intensive, although the masks are inside the chamber for what looks like 8 hours in between bouts of activity. The masks have to be handled and inspected both before and after the sterilization procedure.
Is the labor the reason the contract costs so much? A key missing piece of information is just how long the contract lasts. Recall that the DOD press release indicates that Battelle is providing the labor for the process along with maintenance of the chambers.
After a bit of digging, I found a few more details. Here is information from a Defense News post that is dated April 13 in its URL:
Battelle has already set up two machines in the New York City area, as well as one each in Chicago, Illinois; Tacoma, Washington; Columbus, Ohio; and in the suburbs of Boston, Massachusetts. A solicitation on the organization’s website, found by the Boston Globe, says the group anticipates a need of at least 2,300 workers for 100 sites — or 23 staff per site, which is expected to run 24 hours a day. The $20 per hour job is expected to last at least four weeks.
“We are anticipating a surge over the next two months,” the solicitation read.
Let’s be generous here and extend that two month surge to a full year. If there are 2300 workers each making $20 an hour for a year, I calculate a little under $96 million in direct costs. Being generous again, travel expenses (Battelle in their solicitation mentioned the employees may need to move among sites), benefits, and overtime may bring total personnel costs close to $200 million.
My gut feeling here is that Battelle stands to make quite a bit of money off this contract, even if they run full-out with these chambers for a full year.
But rest easy, citizens. Battelle plans to provide the sterilization service free of charge for those submitting masks and other equipment for processing.





Good bit of investigative reporting, Jim.
From a technical standpoint, I would think that a very high-speed circulating airflow through the containers would help mitigate the problems with the bunching masks.
Lots of multiplications going on here. 20/hour, 2,300 workers, and some unknown length of time. Battelle has never been known to be on the cheap side of contract bids. I would expect in a normal gov’t contract to see some breakdown of administrative costs and profits. I guess the GSA is essentially neutered under the trump/kushner/repuglicon administration.
One of the reasons Battelle is so expensive is that it takes a lot of engineering, planning, and programming talent (all billable) to ensure that there is sufficient distance between contract cost and contract performance.
Thanks.
Efficient circulation and efficient control of the humidity definitely will matter. Way back in the day, I commissioned a couple of environmental chambers built by a local engineer for our insect mass-rearing business. In this case, the vapor and its condensate need to interact with everything on both sides of the mask material, so I still can’t get over how important spacing is. One possibility I’m thinking about is that the photo was staged with those extra rods and that masks don’t really hang like that in the actual process.
And I probably should have made a bigger deal out of not knowing the full length of the contract. I’m assuming the full version eventually will be published, but I wouldn’t be surprised if they’re still ironing out the final wording.
I have no background in science but when you mentioned “circulation” it reminded me of what I thought was an odd story saying the FDA would only give approval for these machine to disinfect a quantity of masks that was substantially less than the manufacturer claimed it was capable of doing at one time. I seem to recall it was about half. The article seemed to be casting suspicion on the FDA possibly foot dragging.
I can’t easily find that story but here is what appears to be pretty transparent support for the company Battelle from a Cincinnati media outlet. https://www.wcpo.com/news/government/state-government/ohio-state-government-news/fda-consents-to-expand-approval-for-n95-mask-disinfecting-technology
Again I am no scientist but I would be curious to know if the FDA’s resistance to what appears to be the quantity of masks the machine could disinfect at one time was removed because they fixed the problem, or because of the company’s ability to lobby?
Who knows. That is an excellent question. I doubt we’ll ever have a real answer.
Here is the approval letter from the FDA
https://www.fda.gov/media/136529/download
Maybe I’m missing something here but why not EtO or e-beaming for sterilization, both methods in routine use for medical devices? Are these ineffective against viruses?
I’m guessing the main reason is that the HPV method was already documented by FDA.
This site by CDC :https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
has a very good summary of the other commonly used practices. It appears that EtO is of concern because of how long it takes for it to diffuse out of the mask material coupled with its extreme toxicity.
Here’s why some other approaches are not allowed: “Decontamination using an autoclave, 160°C dry heat, 70% isopropyl alcohol, microwave irradiation and soap and water caused significant filter degradation to both FFRs and particle penetration levels did not meet the levels that NIOSH would allow for approval. Decontamination with bleach caused slight degradation in filtration performance and created an odor that would not be suitable for use.”
The ETO has been phased out and replaced by these HPV systems over the past decade or two. ETO is much more harmful and leaves a toxic gas behind that has to be vented into the atmosphere. The items in an ETO sterilizer need to aerate for several hours before they can be safely handled/used. The HPV systems like Sterad only need a brief cool down and aeration period, so throughput and turnover times are greatly reduced. I spent the last 25 of my productive years working in a busy operating room, so sterilization issues were always coming up and the technology was constantly evolving.
As someone who routinely will pull recyclable items out of another person’s trash, you’d think I would be thrilled that the Trump organization is pushing this option to clean and reuse a scarce resource that is in high demand.
I can’t quite put my finger on why I am suspicious?
I have to wonder what it costs to disinfect a mask vs the cost a new one.
To be fair we would need to compare the costs before and after Trump’s pirates made sure masks remained scarce.
A big reason why this has to be done is that the producers of N95 masks simply can’t keep up with world demand right now. It seems to be generally understood that once supplies get back under control, the approval of re-use will be withdrawn. But that relies on logic, which is in very short supply among the powers that be just now.
The stated period – one month – does not seem to fit the other terms of the contract. But it would be typical in defense and other government contracting to low-ball certain parameters in order to set-up a sourcing arrangement, then let the duration and volume of purchases balloon. That keeps the apparent but not the actual costs of a contract within politically acceptable tolerances.
Demand for an effective service of this kind will extend for over a year. The new and expensively developed surge capacity needs to remain available for a) a contagion likely to last longer than governments admit, and b) probable recurring waves of infection. Those seem likely until the vast majority of the population develops herd immunity through exposure or vaccines. That immunity will need to be re-established periodically, in order to prevent further recurring waves, as it is maintained now through vaccines for other “childhood” diseases.
That immunity will be threatened by a global South that hasn’t the resources to pay for monopoly-priced vaccines. That gap is partially plugged by international aid agencies, which I believe includes the WHO. (One reason Trump apparently chose not to use the WHO-designed test is that it would have had to pay for them. WHO provides them free only to the destitute.) Scandal resulted, for which Trump is properly to blame. He keeps score about things like that, and getting even is one of his defining characteristics.
Governments now have a choice: invest in and acquire the IP for such vaccines, or let the IP remain in the private sector. If they allow the latter, monopoly and monopoly pricing are likely to result.
I work in an emergency department in Boston where we just got a shipment of these newly sterilized 3M N95 and people cannot wear them. They reek of chemicals that make it impossible to breathe. I wasn’t able to wear one for over 5 minutes. I began to feel dizzy. I can’t imagine this is healthy in the long term.
Wow. Do you know if they were sterilized by the Battelle process for sure? Because that’s really bad news if so. I would have expected this problem for masks treated with ethylene oxide, as discussed above, but if done properly, I was under the impression the HPV should not leave an odor or residue.
Oh my goodness. I’m sorry to hear this, had hoped sterilization process would be a solution.
Wish I knew if a lower temp (165-180F) high pressure (water only) system would work. Hope we find a better answer fast for your sake. Thank you for sharing.
How about e-beam? It’s what we used for a device with gels in it, and doesn’t leave stuff behind like ethylene oxide and hydrogen peroxide does.
I do not know if the effectiveness studies have been done on masks but It cannot be any worse than cartoned medical devices with paper IFUs.
Reminds me when NASA got caught in the 70’s for billing
$960 per for an instrument line itemied as a Multi Directional Impact Generator more commonly known as a hammer.
I’ve always wondered how much of that was for whoever had to write the specs so they wouldn’t get cheated by a supplier who low-balled their bid and provided substandard supplies to make their own profit. (This is a real problem. I worked in a building that cost more than $60K, as much as a good house in that area, and was *definitely* cheaply built.)
A team at Caltech has developed a technique for sterilization and reuse of N95 masks. Please take a look and if you like it pass the word on. http://web.gps.caltech.edu/~jkirschvink/pdfs/nazeeri_kirschvink_n95_mask_vacuum_restoration.pdf
Wow. Interesting finding. And their observations also present a caution for other methods to make sure the masks are dried efficiently. It would seem the Battelle method would be at risk for leaving the filter material wet enough to perform poorly, but they present data in the FDA report showing the filters still working to remove bioaerosols after multiple cycles of treatment. So it’s really difficult to figure out what to make of this.
For what it’s worth, I spent a lot of time around Caltech folks as my wife got her graduate degree there. I trust them to get things right.
Please pass this information on.
That’s encouraging news, especially if the process is cheap.
That such a small amount of residual water negatively impacts the mask’s filtering ability makes me wonder about the safety of the current practice for health care workers to wear one N95 mask continuously for hours at a time. What is the mask’s filtering ability at hour 6 after continued exposure to the wearer’s exhaled (humid) breath?
FWIW, I recall an earlier discussion about vaporizing hydrogen peroxide for sterilizing stuff at home and was warned off it as being very dangerous. Someone in the comments thread (that I can’t find) spoke of a robot that was used to sterilize entire hospital rooms …
Anyway, $415M/60= $6,916,666.67!!!
A few weeks ago the University of Tennessee Research Institute published a paper by the inventor of the N95 mask on cleaning it for re-use. The institute has since removed the paper, but posts this note:
“Due to the extremely fast evolving data, UTRF has removed its FAQ in favor of the consortium site.
For more information on N95 face piece decontamination, please see: https://www.n95decon.org/ ”
That could reflect simply good scientific and medical practice rather than the result of any coercion. Choose your own way to bet.
Here’s a version of the original paper from The Wayback Machine.
And this is the PDF version originally linked in the post.
The Taipei Times wrote about Tsai last week.
Nice read, Jim.
The follow-the-money angle certainly puts into a different light Battelle’s ‘all hands on deck’ attitude mentioned in this article which is mainly a feel good story about how the current decontamination plan came about.
To summarize, on March 13, 2020 a married couple were discussing the growing shortage of N95 masks. Dr. Laurie Hommema works for OhioHealth as the Medical Director of Provider and Associate Well-Being, and her husband Kevin Hommema is a principal research scientist at Battelle .
Dr. Hommema remembers telling her husband she wished the dwindling supply of N95 masks could be reused, and he surprised her when he mentioned the Battelle project from a few years earlier that demonstrated proof of concept to do just.
“Dr. Hommema called her boss at OhioHealth, Dr. Doug Knutson, to tell him what she learned. “I said, ‘Doug, Battelle has the science. They did it! Can I look into it and investigate?’ He said to run with it,” Dr. Hommema said.
The rest was history. Less than 48 hours later, senior leaders from Battelle met with OhioHealth. Within five days, OhioHealth sent the first shipment of PPE to Battelle so they could test the technology they worked on years before.
“That became the number-one priority project in all of Battelle,” Kevin Hommema said.”
link is CBS affiliate in Ohio:
https://www.10tv.com/article/couple-and-conversation-behind-battelles-mask-sterilization-technology-2020-apr
How many times can N95 mask be cleaned with hydrogen peroxide vapor?
The numbers vary.
MGH Brigham Partners’ early press release: up to 30 times (4/03/20 news release)
https://www.massgeneral.org/news/coronavirus/research/partners-healthcare-mask-sterilizing-facility
Battelle website: up to 20 times.
(Only the N95 mask manufactured by 3M was tested several years ago, the model 1860. This 3M mask does not contain cellulose which would dissolve in hydrogen peroxide vapor. Battelle discovered that the elastic strap of the mask elongates and loses elasticity by the the 30th cycle, impairing mask fit.
But, per an NBC news blurb: about 8 times (April 11, 2020)
It is embedded in a sentence that makes it unclear whether MA Gov. Charlie Baker is the one declaring it.
“Between acquiring the shipment and the Battelle machine, which will be able to clean those masks for reuse up to eight times, he [MA Gov. Charlie Baker] said last Friday, “you start to feel like you’re creating a little bit of a comfort for a lot of people who had been uncomfortable.””
https://www.nbcboston.com/news/coronavirus/baker-to-tour-medical-mask-sterilizing-machine-being-readied-for-mass/2106139/
is this dod contract a sole source contract? if so there is probably lots of wiggle room.
recently sec. esper spoke publicly of the dept. beginning to prepare for a possible pandemic in early january. it would be surprising if the battelle contract did not have a connection to that effort.
I was excited about methods for safely reusing N96 masks until a doctor friend of mine sighed and explained that the filtration degraded with hours of use. If you get 4 hours out of mask, then sterilizing it for eight hours between several uses still gives you four hours of use, total. I made a sad noise and gave in.
Honestly, the easiest way to decontaminate them is probably putting them in a box for three days. Also cheaper than this bullshit..
I am stunned that anybody who has ever used the classic N95 thinks that it could be regenerated more than once or twice. Especially via any kind of liquid intervention, whether involving H20 or H2O2. It is absurd.
yeah! and I have worn them. i was trying very hard to think about ways to disinfect them without using harsh chemistry or much heat for exactly that reason. i’m very confused about how this is getting talked about.
kind of makes you feel a little bit like a crazy person. like, is anyone fit testing these after they’re sanitized?
Wow. That observation would fit the Caltech data on masks losing efficiency due to adsorbed water. In this case, it would just be the humidity from the wearer breathing.
Seriously, how could that “not” be the case?? Some of this stuff is just nuts.
I was coming here to answer Quinn Norton’s 1216a Q re fit testing cause I’d already read about it, and it turned into a sidecar project when I found that 3M had login-protected the germane technical bulletin which I’d posted here a few weeks ago. I found an update which begat more questions, so here’s the new journey. (As an aside to Rugger9, 3M in these documents completely rules out EtO due to remnant inhalable toxics, as others noted.)
● 3-26-20 Duke publicized their VHP decontamination study of N95s for reuse, using the Bioquell Clarus C (the same unit in Jim’s post photos and the 2016 Battelle document). Duke also said they performed their “normal quantitative fit testing process” and actually fit tested on “two individuals with differing facial structures with no loss of fit or seal”. _Two_ faces. They had used 100 3M masks in the study (IMO there’s too much missing data in their manuscript: I was looking for more than they included on the post-process. Like a nice table and some parameters on the H2O2 conversion and drying out).
● 3M adds a 3-27-20 statement to their technical bulletin (“March, 2020, Release 2”, document created 3-29-20; clicking link prompts a login request, so no longer available — adding some quotes here), which states that no method has yet met their criteria:
3M Technical Bulletin – Disinfection of Filtering Facepiece Respirators (PDF, 213.93 KB)
https://multimedia.3m.com/mws/media/1816576O/disinfection-of-disposable-respirators-technical-bulletin.pdf
In this document, 3M reviews prior studies and a variety of methods (including VHP) but not the Battelle work Jim linked (the 2016 document). They conclude:
● An update — technical bulletin “April, 2020, Revision 4” created 4-14-20, modified 4-16-20:
Decontamination Methods for 3M N95 Respirators
https://multimedia.3m.com/mws/media/1824869O/decontamination-methods-for-3m-n95-respirators-technical-bulletin.pdf
Here, the document begins with CDC guidance: ideally workers should have five FFRs so each can lay dormant in a brown paper bag for five days between each use. They summarize various decontamination methods, including a number of VHP systems.
So what was weird: they list VPH by Bioquell as “under investigation” for all column data, with no EUA, but have a separate entry, next row, for VPH by Battelle. Of note: while the VPH by Battelle remains “under evaluation” for “Cycle”, it is rated as “Pass” for “Filtration Efficiency” and “Fit Related Evaluation” for three cycles, with 20 cycles “under evaluation.” (They also link Battelle’s 3-29-20 EUA and related docs).
So the “up to 20 cycles” in Battelle’s EUA is basically some live experiment with our medical workers (well, like we needed a document to tell us that). Given issues as already cited in post and comments, is this investment really going to spare N95s vs other methods (besides brown-bagging them, and including making more).
And I thought the row distinctions and naming between Bioquell and Battelle were weird (to be more precise, the Bioquell row states “VHP- Ecolab, Bioquell”, and the Battelle row just “VHP – Battelle”).
Also, Jim, I cringed at the lumped-up masks in that photo, too.
The Duke ms. from which I quoted:
N-95_VHP-Decon-Re-Use
https://www.safety.duke.edu/sites/default/files/N-95_VHP-Decon-Re-Use.pdf
Battelle has been spoiled by decades of being either overpaid or absurdly overpaid for their work, or even – for not doing that work. Back in January, 1995, I was at the annual meeting of the American Nuclear Society in Richland, Washington, where the Hanford Works HQ is. Battelle was basically honored that night for having been able to win a HUGE nuclear remediation contract that pretty much didn’t ask them to remediate anything. The 200 or so nuclear engineers and nuclear industry reps gathered around the banquet tables gave them a whooping minute-long standing ovation.
Ohio…. a swing state.