Michigan Is Using More a Pessimistic Model than the White House
On Monday, the CEO of Spectrum Health, Tina Freese Decker, sent out an update on COVID-19. After explaining how they’re modeling the virus, she said that the model they’re using says our peak (presumably meaning Grand Rapids and environs, not Michigan as a whole) would be in early May.
[W]e are closely studying our models, which include learnings and data from across the state, country and world. These models project the spread of COVID-19 and enable us to estimate how many people in our communities will need hospitalization and intensive care services. They also allow us to understand the collective resources that would then be necessary to serve those needs. These are just estimates and we hope for the best, but our job is to plan for the worst.
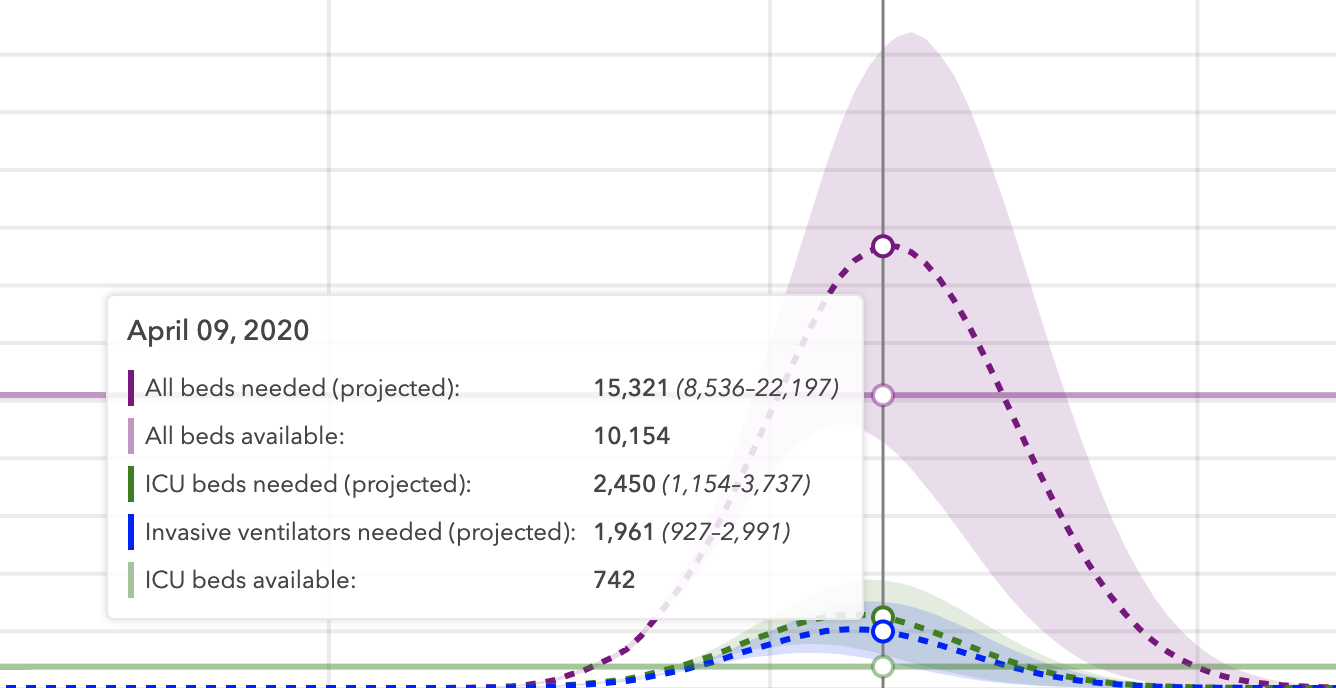
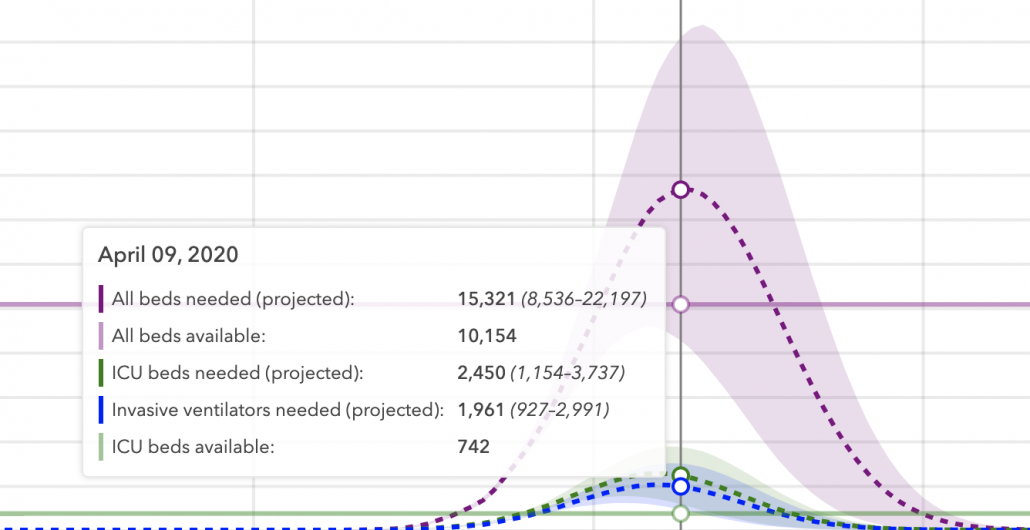
At present, based on the information available, the rate of growth of deaths from COVID-19 in Michigan is at least as fast as New York, if not faster. The modeling for our area shows that, at its current rate, we would exceed demand for hospital and intensive care services in early May and this would last many, many weeks. This peak in cases would be more than our health care system, or any health care system, could handle.
That conflicts with the IHME projection for the state by several weeks.
I thought, at first, that that might just reflect the fact that cases in my county, Kent County, have been increasing at a more gradual pace than in SE MI. That is, it might reflect that our curve is flatter than the state as a whole, and while Kent is the state’s fourth biggest county, the population of those hardest hit county still dwarfs ours.
Except that Governor Whitmer has twice used the same estimate for our curve — early May. In both a press conference yesterday and in a town hall, she and MI’s Chief Medical Executive Joneigh Khaldun said our peak will be a month from now, not a week.
Maybe Whitmer and Spectrum and everyone else are trying to prepare for the worst. Or maybe they’re seeing something in the state-level data that is not making it into the public data IHME is using.
A physician leader at a major academic medical school in the south walked me through some of what the IHME model may not fully incorporate, based on what he’s seeing in a hard-hit city: how long patients are kept on ventilators.
As you know I am exec leadership at a large University Hospital, so I have access to our Covid data.
I suspect one of the factors driving the later projected peaks is related to estimates of time in hospital. While some non-critical patients are admitted and discharged over 3-7 days, the ones admitted to the ICU are taking much longer to move.
The peak of detecting infection precedes the peak need for hospitalization by 7-10 days.
If you look at the IMHE data, their curves for hospitalization and need for ICU and ventilators are temporally aligned. I think this is going to be very wrong.
The issue is that once a patient is in the ICU or on a ventilator, they stay for a very long time, remaining on the ventilator. Since mid-March, we have intubated numerous patients. 10% have been extubated, 20% have died, and 70% remain intubated and are still parked in the ICU.
Thus the peak need for ICU/Ventilator curve should probably be pushed back several weeks as the tail end of the infections will just accumulate more ICU/vent need in the weeks subsequent to the infection/hospitalization peaks. I suspect the local governments are figuring this out, and the math guys at IMHE have not plugged this factor into their models yet.
The burden on health care capacity will persist long after the infections abate- necessitating much longer control measures to avoid and reemergence in volume.
If this is right, then it may reflect differing goals. Whitmer and Spectrum Health need to identify how many ventilators they’ll need for how long, whereas the federal government needs to identify how long it’ll take to get the first wave of people who’ve contracted the virus either into hospitals or through the period of contagion. Though if that’s right, it may explain why Jared Kushner and others at the White House think governors are exaggerating the number of ventilators they need: because Kushner isn’t accounting for how long a patient stays on a ventilator.
But if Michigan is right and IHME is wrong, it matters that the White House has largely endorsed the IHME model. Even ignoring the possibility that IHME is not sufficiently accounting for the time patients spend on ventilators, there are parts of the projections that do not match reality. The IHME model assumes every state will have a stay-at-home order, but a bunch still don’t and the White House recommendations still fall far short of that. The IHME model assumes everyone will remain on stay-at-home until June (an assumption it made far more prominent on its site after the White House endorsed the model), but Trump promised it would be just 30 more days. While IHME uses deaths to project the curve — justifiably treating that as a more reliable measure of COVID rates than tested positives — there’s reason to believe that even death rates are unreliable (for example, some areas are showing spiking pneumonia deaths not otherwise attributed to COVID-19).
As it is, Trump promised that everything would start to get better in two weeks (though later in his presser, he admitted it might be three weeks). He did so while falsely suggesting that the IHME projections match the recommendations of his White House, which they don’t.
But if hard-hit states like NY (for which IHME has already significantly adjusted its model) and MI are as much as a month out from peak, then Trump’s rosy projections could, once again, lead to recklessness.



I think second guessing the assumptions of models like IHME about the degree of national isolation is the right explanation for what Michigan is doing.
I suspect there is also skepticism about the ability of the US to implement more sophisticated testing and limited isolation once we are past the initial crest. They are anticipating the possibility that this won’t be a bell curve but a series of waves.
The model seems FUBAR when it comes to resource projections. It says New York needs 60,586 hospital beds today April 3. Cuomo said the hospitalization was 13,393 and ICUs used 3396. Covid tracker says 20,817 beds cumulative, so current does not count released or dead. The model keeps saying New York only needs about 9,300 ventilators. Cuomo has been asking for 40,000.
Apologies to the model creators. I know how tough it is to do. Bad things happened when people took my work before it was completed and checked.
Anyone running with this models resource estimates you are warned again here and now.
Ominously, propublica just began examining racial factors in several locations. Quote: “In Michigan, where the state’s population is 14% black, African Americans made up 35% of cases and 40% of deaths as of Friday morning.“
I’m usually the first person on top of the issue of race here but I think this is a partial misread of the situation.
Detroit Metro Airport (DTW) is the 10th largest U.S. airport and the 18th busiest with 36M passengers in 2019. It serves international traffic and it’s a Delta hub. Guess how many employees at that airport are black and live in the Detroit area…I think I’ve read the airport authority has 500 employees, but I don’t have any percentages wrt demographics. I’d bet the demographics mirror Wayne County where the airport is located.
Also need to keep in mind (2) federal TSA workers tested positive for COVID-19 on March 24. They probably were exposed within the previous two weeks and contacted a LOT of both federal and DTW employees before the tests’ results were available.
What’s NOT a misread is how Trump responded to aid for Michigan and by extension, Detroit. Race and misogyny have a lot to do with his bullshit failure to do his job.
Thanks. Did not know about the airport worker risk. What do you think the issue might be in Milwaukee (also a big part of same story). Urban poverty, health disparities? Access to healthcare?
Possibly. But the part of Milwaukee with most cases is not only more dense in terms of black residents, but a higher concentration than average of universities and colleges. These schools are within a 5.5 mile radius:
Milwaukee Institute of Art and Design
Herzing College
DeVry University
Milwaukee School of Engineering
Marquette University
Concordia
There’s a lot more young carriers, if I had to guess.
I wonder how many from western Ontario use Detroit as their airport.
I noticed an alarming difference in observed mortality rates in the NY Times Coronavirus case/death counts
https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html#states
NY has a 13.5% death rate, NJ 6.1%, MI 4.2%, and LA 6.6%. This is far above the <1.0% death rate for most other states. Is that just poor access to health care, higher co-morbidity, and slowness in effective response?
Testing and timing probably are at play. We are not detecting the barely symptomatic and asymptomatic cases. And we are also not detecting the deaths that normally would have been averted. Our data streams are poor at the moment.
The differences in mortality rates could easily be an artifact of testing/diagnosis.If you are calculating death rate as a percentage of those testing positive then the fewer you test, the higher the calculated rate.
Alternatively it could be real and reflect how far demand for ventilators (and other care) has exceeded supply.
Either way I don’t see how a rate that doubles every three days leads to only 200k deaths in two weeks, it should be at least twice that unless something slows it.
I find no reason for such optimism unless its to keep people from panicking.
I’m sorry, my bad. That number is not % but deaths per 100,000 people (in population?). That seems like a useless measure, compared to mortality as % positive. Guess it may be roughly a measure of level of undetected infections out there.
Pajaro:
I am a bit confused. The NYT date you link to says 102,870 cases and 2935 deaths. That seems to be under a 3% death rate not 13.5%. Am I missing something?
I agree with both of you. Waves instead of a smooth bell curve. Each state will have its own wave forms and some will be disruptive both within states as well as across states. Success in ventilator treatment and length of time in use will vary a lot even assuming they are freely available. That BBC article I put up yesterday about how different models deal differently with variables is useful.
This doctor, Duc Vuong, reached the same conclusions. People who get entubated stay alive for many days, but have poor outcomes. Morbid obesity, his patient group, are at very high risk.
The peak of mortality and ventilator use will follow the peak of active cases, by 10-14 days, and the detected cases have not peaked yet.
I’m in the Muskegon area and I am shocked how much manufacturing is going on. Add in transportation/distribution and then retail like groceries, C stores and Lowe’s etc. and the economy is very far from shut down here. The first cases were late arriving here and I fear a huge spike in coming weeks. Hope I am wrong.
I’m worried abt Muskegon, too, bc it has the same underlying health problems that made Detroit so vulnerable.
And yes, manufacturing has far from shut down.
Patients are given sedatives and anesthetics, and, sometimes, paralytic drugs when they are intubated and also continue to receive sedatives and pain relievers while they are on ventilators. The necessary drugs are in critical supply. There simply may not be enough of them to get people through this crisis. I wonder if any of the models are sensitive to this issue. Of course, there also is the issue of having enough trained people to care for ICU patients on ventilators.
If I remember correctly, Oakland County had run out of sedatives and pain meds more than a week ago. We’re also seeing a lot of health care workers getting sick and in too many cases dying, though I haven’t seen this in Michigan as much as I have in New York.
The wave is not just higher but wider at the front edge as well as the back.
I wonder how many of the general public (and some Southern governors) hear the word “intubated” and imagine something like a glorified CPAP machine. There are videos on YouTube describing how the reality is far different and what all is involved–the sedation; the physical restraints; the need for frequent oral care; the suctioning up of various kinds of crud; and, of course, you don’t just get up and take a stroll to the washroom when the need arises. People might be more willing to commit to social distancing and staying at home if they had a better idea of the ordeal they or their loved ones might face if they fall sick with COVID-19.
From a modelling perspective, calculating the sedative and pain relievers needed appears to be a relatively straightforward thing to do. “We need X amount of drugs for a duration of Y days per patient, then multiply by Z patients . . .”
Models rarely attempt to track every possible data input, but different models examine different things. The other big measurable item I wonder about is people: doctors, nurses, techs, lab folks, etc. This is perhaps the most difficult item in this situation to model because we’re just starting to figure out the rate at which staff will become exhausted, exposed and required to quarantine at home, exposed and require hospitalization, burned out totally, or deceased. Some may be able to return after time away, while others will be dead. Then there are the possible additions to staff, by bringing retirees back to the hospital, advancing the training of med students at the end of their program, and bringing in staff from other states.
It’s possible to model these things, but the range of possible values to put into your model are very very wide.
Emptywheel: A Question
Does anyone have an idea how the Michigan outbreak started? Has there been any contact tracing?
I’ve heard local leaders say that they expect to run out of ventilators in New York and the greater New Orleans area some time early next week, so we’re about to see what happens when you start crossing one of those lines on the chart. I’ve heard one intensive care doc say that they’re worried that where they are, they may run out of dialysis machines before they run out of ventilators, which would throw renal failure into the mix as a possible killer. Questions that I think are going to come up that I haven’t seen anyone address:
1. Everyone knows that we’re going to have a “life boat” problem (or a “trolley problem”, or whatever your metaphor of choice is), and people are going to have to decide who gets a ventilator and who doesn’t, which is more or less a decision about who lives and who dies. I’ve heard people say things like, “We’re not going to discriminate based on age or disability.” Okay. But what ARE we going to discriminate based on? We either have to come up with national or state-level decision trees, or we’re going to have to let the hospitals decide for themselves. Yes, we have to triage people all the time during emergencies, but never like this. Our health care workers are already emotionally exhausted. This is just going to shatter some of them, and every decision will be second-guessed by both the people who made it and by outsiders that include not only friends and family, but also politicians a media “experts”. We are NOT ready for this, and the conversation needs to happen NOW.
2. Every nerd in the country (including me) has some idea of how to make a jury-rigged ventilator. The FDA is going to be under enormous pressure to approve many of them, but none of them will be nearly as sophisticated as a “real” ventilator, and I’ve seen intensive care docs say that some of these would probably work for some issues but not for others. (All of the docs I’ve talked to have said they’re not going to work for acute respiratory distress syndrome (ARDS), because the patients are so fragile that the vents constantly have to be “fine tuned” as the disease evolves.) So now we have an additional variable that goes into our triage problem. Who gets which ventilator? This another conversation that we need to have NOW.
3. Ventilators (and some other major equipment) are going to have to be moved around on a large scale based on where they’re needed. No one in any hospital is going to want to let go of any of their ventilators. So again, another triage problem. The vents that you’re moving may be needed at their original location in 10 days based on some models, but in 30 days based on others. If each patient at the destination hospital needs a vent for 20 days, you have a problem. You’re now triaging equipment as well as patients. Doctors and nurses aren’t used to doing this, and they’re going to be biased based on which hospital they’re at. Who decides which ventilators go where? Governor Cuomo is starting to have to deal with this within New York State, but it’s eventually going to have to be done at a national level. Someone is going to actually have to move the damn things, too, and that’s not going to be a trivial job. You’re going to need to move them without breaking them, and I doubt you can just put them back in the box and be ready to go. Who’s going to co-ordinate all of this? Jared?
Apologies for the length. Feel free to delete.
Michigan’s Henry Ford Hospitals faced the question of triage a week ago, publishing a letter which outlines their decision process. The letter is provided to patients at intake so they know what the criteria are before they are told you won’t be put on a ventilator.
I’m sure the actual decision process is a bit more detailed, with scoring assigned during evaluation. But the ‘death panels’ are already operating where resources are limited.
And the person who makes the decision affecting the most patients, effecting the most deaths because he refuses to ensure adequate PPE, beds, and ventilators are in place? Donald fucking Trump.
‘This is just nuts’: COVID-19 pounds northern Michigan county
https://www.detroitnews.com/story/news/local/michigan/2020/04/03/covid-19-pounds-otsego-county-coronavirus-pandemic/5093984002/
Craig Mauger Published 2:36 p.m. ET April 3, 2020
The churchgoer who went on a mission and picked up the virus during his travels may have infected more people if he went to church but I don’t see that in the article.
The nugget in that article is the second home phenomenon:
Yeah. That would explain the spike, lots of folks who might ordinarily only show up in the summer for golf or only for the occasional winter trip are bunkered down away from their homes in more densely populated areas.
There was a nice piece in BuzzFeed this past week which explored this effect: This Pandemic Is Not Your Vacation.
Makes me wonder if one of the ‘hidden’ pieces of data informing Michigan’s Gov. Whitmer about the duration of this wave of contagion is the number of non-residents now in state as well as travel numbers for persons who’ve flown in/out of Michigan from places which don’t have Stay-Home orders or have high infection/death rates. Not certain how she’d obtain such numbers but I can think of a few methods if I tried it myself.
In Ohio today, Gov. DeWine and Dr. Acton stood behind the modeling done by Cleveland Clinic, the State Department of Health, and Ohio State Univ., all of which are more conservative(?) in their assumptions, and which show more and longer cases than IMHE. They try in the most oblique way to disagree with the Trump, but they obviously believe that they’re right an IMHE is wrong.
Also, noted biostatistician J. Kushner is full of shit and we’d all be safer if he’d just STFU.
If widespread testing was available it would identify those who had mild cases of Covid 19 have recovered and are no longer contagious. Such people could then be working/volunteering (instead of locked down) without fear of catching or spreading the disease to those still vulnerable. Is this the success behind S Korea’s ability in returning to normality?
I don’t think so. On April 3, South Korea had 10,156 cases, of whom 6,325 had recovered. That’s several orders of magnitude less than what would be needed for herd immunity. Their success is much more likely to be due to aggressive testing and contact tracing. If you get right on it quickly and pour resources into it, you can find and isolate all contacts before there are too many to handle. Unfortunately, it’s too late for that in the US.
How long they stay on ventilators. That is the question. Before we had the polio vaccine we had an outbreak of polio in BC. the summer before I started grade one. I remember the iron lungs and they were not a temporary measure. Some remained in them for very long time. While we are going through this pandemic my memory goes back to that time remembering kids whose parents died in our community. I also wonder what will happen if people can’t come off those ventilators. In Canada I know the TB hospital in Vancouver became the iron lung hospital but what will
Happen in the USA
It’s wierd how things of over 65 yrs come back. I know we got through that so I hope we will get through this
@ e.a.f.
“Workers at the Harmac Pacific Mill in Nanaimo on Vancouver Island, BC, Canada, are working overtime these days producing the special K10S pulp used to make N95s and surgical gowns because a U.S. manufacturer that produces the things has recently doubled its order.” https://www.vicnews.com/business/nanaimos-harmac-mill-works-to-fill-doubled-pulp-order-for-medical-masks-and-gowns/
Thank you for mentioning that. Dix, Minister of Health BC mentioned it on the news yesterday. The mill isn’t that far from our current home. Our previous home in Nanaimo was closer and some times the prevailing winds also brought the “odour “. My line was always shut up that’s the smell of pay cheques. It isn’t going to kill you
It was so silly for trump to try to order 3m to not honour orders. We need to share. Just as China sent equipment they no longer required to Italy. Yes your own country comes first but not at the expense of common decency
Had the trump administration handled this in a better manner things would be better. What amazes me is the cabinet it whomever hasn’t made a move to remove him. Many are playing up to his vanity but their citizens are dying
Nanaimo is a great place. Has a nice small university. Diana Krall is from here. Pamella Andersen lives 20 min down the road in Ladysmith which is gorgeous. Incredible views old buildings. It’s nice here on Vancouver Island. Great place to send your kid for university if they aren’t ready for the big ones. Beaches sorry I’m starting to sound like the Tourism dept
The people at Harmac have kept the town going through thick and thin
The things that have “bothered” me in all these models is whether they account for (I doubt it) the infection/burnout of the front-line medical workers treating these patients.
Yeah, there’s talk about recovered medical workers being immune and back on the job, but they also probably suffer the same disease durations and outcomes, unfortunately including death – there have been too many of those already.
And aside from military equipped/staffed field hospitals where are the personnel going to come from to service the thousands of temporary beds that have been and are being built?
I do believe the idea of a nationally mobilized medical team with equipment – like Cuomo proposes – makes a lot of sense. It would give burned out workers a bit of a break and rotate those “waiting” in to get experience. This every state/community for itself makes absolutely NO SENSE.
Pete
The President’s double standard: With regard to himself, the COVID-19 pandemic is an unprecedented event that no-one could have foreseen. With regard to state governors, they should have been prepared for this and made sure they had adequate stockpiles of medical supplies.
The White House models, including Fauci’s, have been optimistic from the beginning. We’re gonna be on triage for months in some states.
A lot more coverage should have been given to the Mueller report when it clearly stated Trump can be charged when he leaves office. Right now he’s using ventilators and N95 masks as bargaining chips for states he needs for reelection. This is happening and it’s getting very little coverage outside our bubbles